The information below and in the related links is designed to help you understand what your A1c reading may mean for your health. However, this isn’t a substitute for medical advice, particularly since a number of individual factors may influence your blood sugar. Please discuss your concerns with a doctor or medical practitioner.
What A1c Scores Mean
The A1c test measures blood sugar over the last three months by looking at the percentage of hemoglobin (red blood cell protein) saturated with sugar. An A1c of 6.2 means that 6.2% of the hemoglobin in your blood are saturated with sugar.
When a certain percentage of your hemoglobin is coated with glucose, it indicates that the insulin hormone in your body isn’t properly removing the glucose from your blood.
A1c readings aren’t strongly influenced by how long ago or what you recently ate. Instead, the A1c test gives a better indication of your health based on information over a longer period of time. It’s able to do this because red blood cells live for approximately 120 days.
Doctors use the A1c test to diagnose type 1 and type 2 diabetes. After diagnosis, A1C scores are used to measure how well a person is managing their diabetes.
The A1C test is also known as the glycated hemoglobin, glycohemoglobin, glycosylated hemoglobin, hemoglobin A1C, Hb1C and HbA1C.
A1c Levels
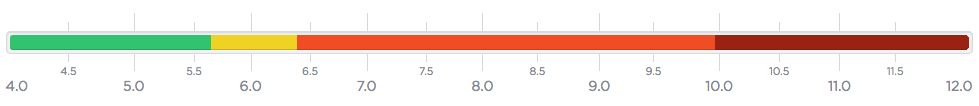
Use the A1c chart and ranges below to help understand your A1c reading.
Use our A1c conversion chart to easily convert your A1c reading into average glucose levels.
Normal
|
A1c Range |
Summary |
|
4.0 – 5.6 |
Congratulations. A1c readings between 4.0 and 5.6 indicate that the level of glucose in your blood is normal. Click on your A1c score to learn more about what your A1c reading means and what you can do about it. 4.0, 4.1, 4.2, 4.3, 4.4, 4.5, 4.6, 4.7, 4.8, 4.9, 5.0, 5.1, 5.2, 5.3, 5.4, 5.5, 5.6 |
Prediabetes
|
A1c Range |
Summary |
|
5.7 – 6.4 |
A1C readings between 5.7 and 6.4 indicate prediabetes, which puts you at risk for developing diabetes. While there are no signs or symptoms of prediabetes, the damage diabetes can have on your heart, blood vessels and kidneys may have already begun. This doesn’t automatically mean that you will get diabetes. However, you should focus on reducing your A1c score and improving your overall health. Click on your A1c score to learn more about what your A1c reading means and what you can do about it. |
Diabetes
|
A1c Range |
Summary |
|
6.5 – 10.0 |
An A1C between 6.5 and 10.0 indicates diabetes. You may already be experiencing symptoms of diabetes, which include increased thirst, frequent urination, general fatigue and blurred vision. Diabetes is a serious condition. Left untreated diabetes can lead to heart disease, stroke, nerve damage, blindness, kidney disease and amputation. Click on your A1c score to learn more about what your A1c reading means and what you can do about it. 6.5, 6.6, 6.7, 6.8, 6.9, 7.0, 7.1, 7.2, 7.3, 7.4, 7.5, 7.6, 7.7, 7.8, 7.9, 8.0, 8.1, 8.2, 8.3, 8.4, 8.5, 8.6, 8.7, 8.8, 8.9, 9.0, 9.1, 9.2, 9.3, 9.4 |
Diabetes (Severely Elevated)
|
A1c Range |
Summary |
|
10.1 – 12.0 |
An A1C between 10.1 to 12.0 indicates diabetes. Not only that, but your blood sugar is severely elevated. This is a dangerous condition that puts you at risk of kidney failure, stroke, nerve damage, blindness and heart attack. The amount of glucose attached to your hemoglobin has thickened your blood. This makes it more difficult to circulate blood through your body, putting considerable stress on your heart and blood vessels. You are likely experiencing symptoms of diabetes, which include increased thirst, frequent urination, general fatigue and blurred vision. Left untreated, hyperglycemia (high blood glucose) can also cause toxic acid to build up in your blood and urine and even lead to a diabetic coma. Click on your A1c score to learn more about what your A1c reading means and what you can do about it. 10.1, 10.2, 10.3, 10.4, 10.5, 10.6, 10.7, 10.8, 10.9, 11.0, 11.1, 11.2, 11.3, 11.4, 11.5, 11.6, 11.7, 11.8, 11.9, 12.0 |
